PSP Overload? Why Fewer Standalone Digital Patient Support Programs Would Help HCPs
Pharma often launches a standalone digital PSP to accompany its drugs, most of which are unused and unmaintained. Here is why fewer patient support programs would help healthcare professionals understand them and, subsequently, increase usage

- Despite failing to gain user traction and acceptance, pharma continues to roll out drug- and disease-specific digital programs that soon become obsolete
- The sheer volume of digital PSPs available makes it impossible for HCPs to keep track of them
- By building on MyTherapy, pharma can tap into a userbase of millions, support patients’ daily needs, and offer drug- and disease-specific modules – simplifying life for HCPs
Digital patient support programs (PSPs) have become an accepted and expected part of modern healthcare, with apps and software supporting patients taking regular medications. However, over the years pharma has launched countless different apps, many of which are specific to certain medications. Not only are these apps lacking in functionality, they typically fail to gain user traction and are rarely updated. With so many PSPs out there that offer little value to patients, is it any surprise that HCPs have neither the time nor inclination to learn about each one and what they do? Here is how pharma can launch effective PSPs for any disease or drug, without overloading HCPs.
Pharma Launches Too Many Drug-Specific PSPs
In most cases, building an entire digital patient support program for a single drug is not only expensive and time-consuming, but it’s also completely unnecessary. Since launching MyTherapy in 2013, we have seen significant patient populations grow for practically every chronic disease.
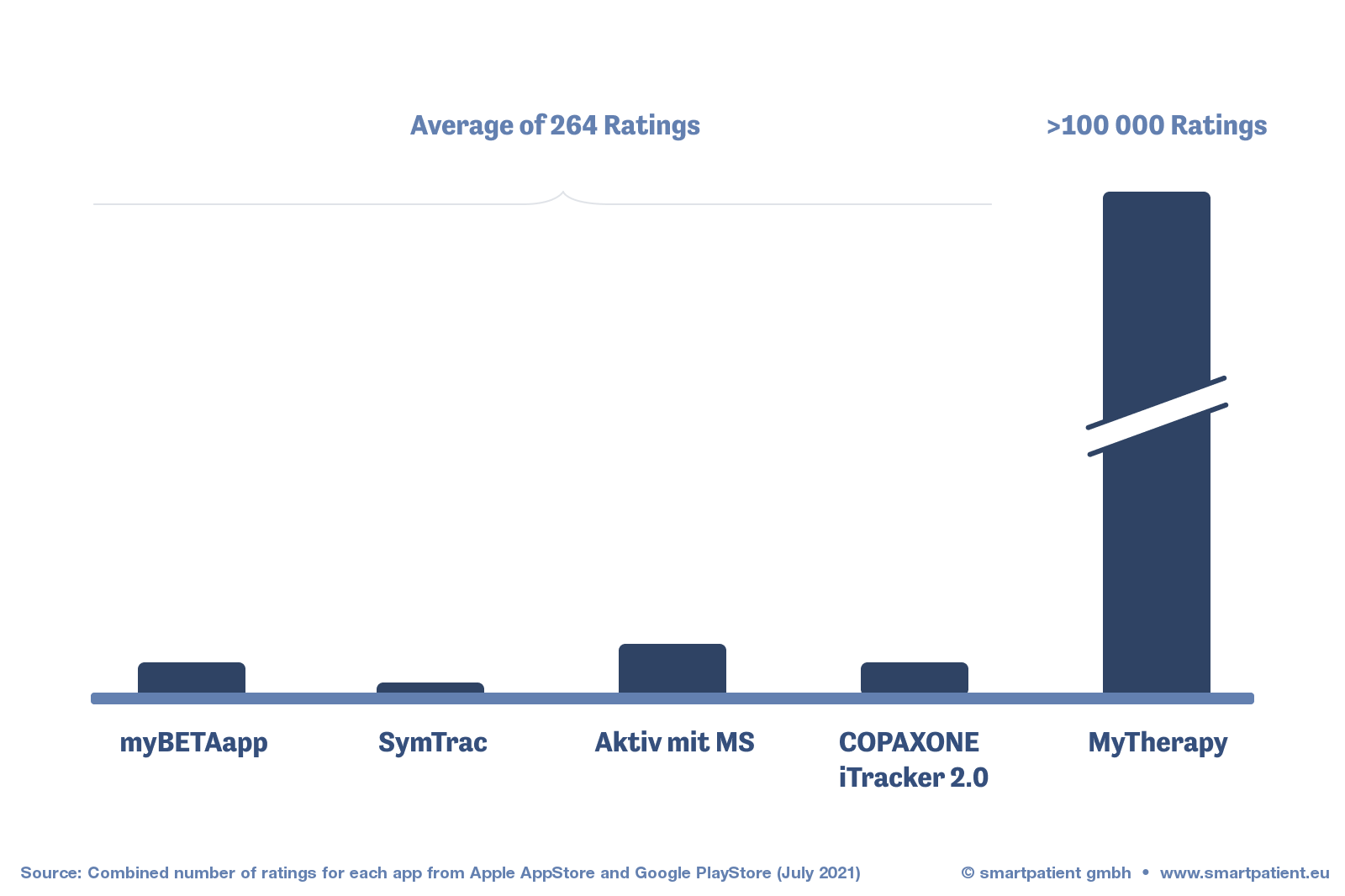
We see that any given drug a patient takes is only one aspect of their daily health requirements; typically, those users also take other medications and often use other features, such as symptom tracking or activity reminders. Despite this, pharma has continued to pump out a plethora of drug- and disease-specific programs. They usually fail. They are too narrow in their scope to be useful to most people, while the impracticality of maintaining so many different apps means the majority receive few updates, if any at all. It’s a phenomenon that we explored in a previous post regarding multiple sclerosis, but one that is prevalent across disease areas.
It’s taken years of monthly updates to get MyTherapy to where it is today; iterative improvements are a fundamental principle of software development.
Even if pharma were to release an excellent patient support program that truly meets patients’ daily needs, how are healthcare professionals supposed to know? The abundance of apps launched over the years makes it impossible for HCPs to know which ones are worth recommending to patients. As a result, fewer patients are likely to learn about the programs, the userbase remains small, and pharma has no incentive to maintain them.
It’s a cycle that fails to benefit pharma, patients, or HCPs. So why persist with it?
Fewer PSPs Means Better Quality, More Users, and Fewer Headaches for HCPs
Simplifying the landscape when it comes to digital patient support is a no-brainer. Rather than building PSPs from scratch for any given drug, we believe a more practical and sustainable model is to build tailored modules that can run on a platform that provides the basic functionalities that patients need.
This is why we consider MyTherapy to be ‘The Operating System for Patient Support.’
For pharma, it is a far more efficient model for launching digital patient support that results in a higher quality product. With the MyTherapy OS taking care of supporting patients’ broad daily health needs, resources can be directed towards ensuring that the modules meet specific needs (including, if necessary, Medical Device capabilities).
Aside from benefitting patients, this model simplifies life for HCPs, who don’t need to waste time they don’t have trying to understand countless different apps.
MyTherapy for [Disease]: Taking it a Step Further
As discussed, the core MyTherapy program has been developed over the course of hundreds of iterations and has millions of users around the world. The app already boasts significant traction across therapeutic areas – typically far beyond the number of users that pharma’s drug-specific offerings have gained.
Despite meeting users’ broad health needs, we saw the opportunity for MyTherapy to offer more tailored support for people living with certain diseases. This is why we have launched a series of disease-specific modules on MyTherapy, independently of our pharma partners. These include:
- MyTherapy for MS
- MyTherapy for Psoriasis
- MyTherapy for Asthma
- MyTherapy for HIV
- MyTherapy for Rheumatoid Arthritis
If we consider MyTherapy to be the Operating System for Patient Support, these modules are like native apps that any user can enable. For pharma, we can run additional drug-specific layers and run educational content and awareness campaigns, offering the tailored digital support that pharma has tried (and failed) to deliver to patients on a drug-by-drug basis.
The result? For pharma, a patient engagement platform with user access and adoption built-in. For patients, access to disease- and drug-specific features on a program that supports their daily health needs. And for HCPs, a simpler, more effective ecosystem of patient support programs that they can trust to support their patients – regardless of which medication they take.
Sounds interesting? Get in touch to speak to us about how MyTherapy can help you support your patients and make the lives of HCPs that much simpler.





