Interview: Moving Beyond Behavior Change Theory to Improve Outcomes
The right message, in the right voice, at the right time: Read how our behavior change team combines behavioral science and editorial excellence to deliver effective content-based interventions

In healthcare ‘patient content’ is often underrated. While there is a consensus regarding the importance of patient education, the potential for effective content to induce behavior change is hardly recognized. And while there is no shortage of agencies crafting content for doctors, only a few can get the ‘patient voice’ right.
At smartpatient, we are convinced that effective, content-based interventions are a key component of any digital therapeutic or patient support offering.
Behavior change theory is our preferred tool for identifying effective interventions. However, no less important is editorial excellence to ensure that content effectively resonates with patients. Our approach to content development therefore relies on our behavioral scientists working hand in hand with our editors.
We've spoken to two core members of our behavior change team: Ellie, a behavior scientist, can call on experience in researching topics relating to chronic diseases, behavior change, mental health, and community health programs. Philippa, a former Medical Editor at Oxford University Press, brings deep expertise in patient-directed contents. Read the interview below to gain deeper insights into their work.
Ellie, what are some of the key elements that underline the theory of behavior change concerning patients living with chronic diseases?
Ellie: When we are talking specifically about chronic diseases, it’s good to remember that a diagnosis often means long-term management and lifestyle changes for a person. In this population, key elements including a patient’s abilities, motivation, and resources are in dynamic interplay. That dynamic varies by individual, type of chronic condition, and treatment.
As an example, consider a pill versus an injectable medication. For someone without swallowing difficulties, the pill may be quicker and easier to take but also easier to forget. The injectable, which requires practice and perhaps generates anxiety, may not be forgotten but avoided. Therefore, we use a variety of behavior change concepts like habit formation and associations in our interventions for patients with chronic disease.
Finally, in the context of chronic disease, it can be helpful to remember that patients experience not only the outcomes of a theory-based intervention but the process of change itself. Addressing both experiences can be part of an “empathetic”, targeted solution.
Within a group of people living with the same condition or taking the same treatment there will still be a lot of diversity. How does behavior change theory apply to people among different demographics?
E: We use qualitative and quantitative research, as well as treatment guidelines to address both the diversity and commonality of the patient experience. Patients within the same indication or treatment group often benefit from an underlying set of behaviors, like attending follow-up appointments or properly administering a medication. They also self-report some of the same treatment barriers that cut across demographics. Research statistics help us determine which barriers are most relevant to target and among whom. Digital health solutions allow for further personalization based on volunteered user data which can be used to set up or adapt a behavior change intervention.
Patients are often more adherent to treatment in the beginning but then drop off over time. What evidence is there that behavior change programs, specifically digital ones, can address this issue of persistence and provide long-term benefits?
E: It’s an interesting question because we are still on the frontier of behavior change plus digital intervention research. Behavior change interventions themselves have been around for decades and target different components of a treatment plan like medication adherence, diet, and physical activity. But that combination of behavior change and digital is a newer science.
So, the benefits of digital interventions have been demonstrated in randomized controlled trials. Regulatory bodies in some markets use RCT evidence as the basis for certain digital certifications. We will learn more about digital interventions’ long-term impact with longer patient follow-up and monitoring, as we would with a new medication on the market.
In the meantime, recently developed tools like the App Behavior Change Scale can be used to predict an app’s behavior change potential based on factors like the inclusion of behavior change techniques, which we use quite intentionality at smartpatient.
Philippa, how do you take the elements of behavior change theories discussed by Ellie and generate real-world value from them?
Philippa: When it comes to content for digital patient support, applying behavior change theory adds value by elevating content to become a potential driver of adherence and persistence, rather than simply patient engagement.
We can also be confident that we’re introducing value by building on the success of relevant interventions we’ve researched and replicating proven solutions.
Returning to the issue of diversity, how do you find a ‘patient voice’ that speaks to as many people as possible?
P: This seems obvious but it’s amazing how easy it is to get it wrong. Firstly, you need to be empathetic and respectful to patients; you want to use language that is simple without being patronizing, especially when you’re explaining elements of treatment that are perhaps scientific or complex; and another point is that if you have the opportunity to bring in other patient voices, that is the most authentic way of communicating and discussing the issues that many of them experience.
Medication nonadherence is a multifaceted issue. In terms of providing content, what types of topics can help improve adherence?
P: Literature suggests that reasons like perceived risk and necessity of medication can differ substantially between intentional and nonintentional adherence groups, which can guide educational topic selection.
Many patients report a lack of time with their healthcare providers to receive sufficient medication education.
Access to social support, management of side-effects, and reducing the perceived effort of taking treatment are all relevant topics when it comes to adherence.
Apps are available to patients 24/7 and can be really valuable in supplementing HCP-provided education along the patient journey.
Financial and insurance concerns are often quoted as leading causes of medication nonadherence. To what extent does this limit the potential a behavior change intervention can have?
E: Affordability of medications and insurance issues vary from market-to-market, so we can’t generalize behavior change strategies and impact globally. Instead, we gather as much research about a market as we can when designing an intervention.
P: It’s also too simplistic to say we can’t tackle issues like insurance with education because it is sometimes a case that patients are unaware of the support that is available to them with the cost of treatment. Additionally, you can make patients more aware of the benefits of the treatment and the potential to reduce medical costs in the future.
A patient’s care team often comprises of doctors, nurses, perhaps caregivers… who is best placed to provide these behavior change programs and why?
E: Barriers to treatment adherence can arise at various points along the patient journey. The care model in the local setting will in part determine who is trained and available to provide behavior change programs.
The relevance of and demand for these programs is likely to grow with the rising global burden of chronic and lifestyle-related diseases. The World Health Organization shared estimates that 60% of the global burden of disease would be chronic in 2020. Effective digital interventions could help address the demand and service gap by facilitating accessibility, with additional content and convenience. So, while digital health solutions aren’t a silver bullet, we see them as something that can supplement HCP interactions.
When it comes to the actual process of turning theory into practice, what sort of approach do you take?
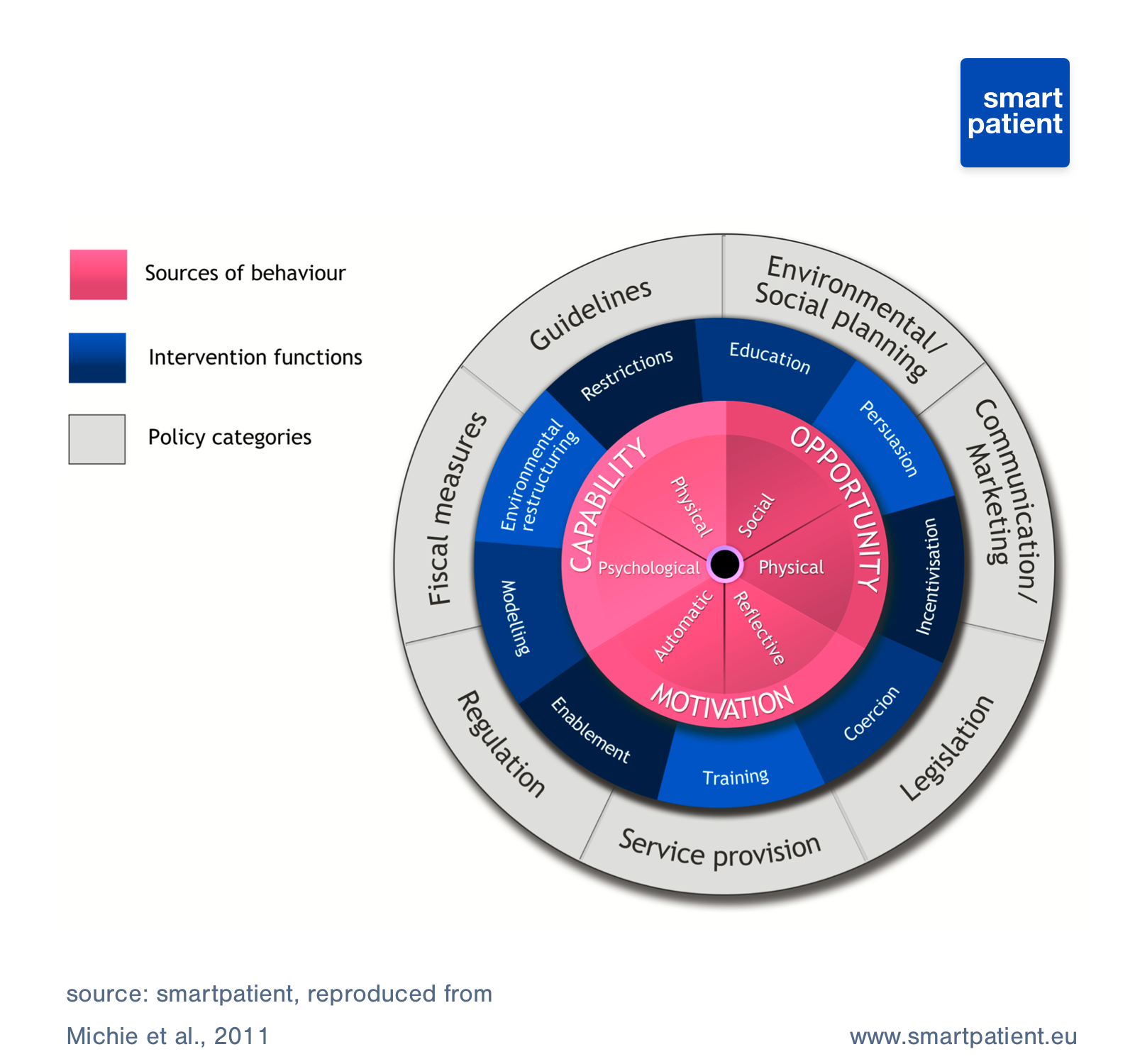
E: I would describe our approach and resulting method as evidence-based and transparent. These two principles facilitate collaboration, trust, and impact. Aligning our method with expert recommendations in the literature was a clear approach in terms of both science and business operations. It does not make sense to completely “reinvent the wheel” when tools like the Behavior Change Wheel and other frameworks already exist to guide intervention design.
We considered these existing frameworks, the digital health context, and company workflows when developing our method. As a result, we can answer both the question, “What is your method,” and the equally valid question “Why is this your method?”. The three-step method we ultimately devised is systematic, replicable, and intuitive. It can be easily communicated to our partners. It also facilitates internal collaboration among smartpatient team members with different areas of expertise.
A black box method would have cut valuable voices out of the design process. People cannot question what you do if they do not understand what you do.
As innovators and scientists at smartpatient, we encourage questioning and build it into internal processes.
Our three-step method gives structure to those discussions. Finally, taking an evidence-based and transparent approach allows for documentation in research studies and increases the likelihood of impact.
You mentioned a three-step method, can you explain how your role related to this?
E: Steps one and two in the intervention design process are most relevant to my role as a health and behavior scientist.
In the first step, I identify barriers to adherence, using scientific, medical, and patient resources. In the second step, I use behavior change theory to derive underlying reasons for nonadherence and specific behavior change techniques to address them. I translate those techniques into practical intervention ideas that our writer, Philippa, can convert into content.
P: So, I then analyze the intervention ideas that Ellie mentioned. That’s a collaborative process and together we decide which ideas make the cut. I then figure out how these ideas can be integrated into content pieces and what the underlying key message needs to be to drive behavior change.
I also have to think about what works well with a timed delivery when we are talking about personalized content that is pushed to the patient at a specific point in time. I then draft headers and summaries and lay them out on a timeline, which we then review with the partner we’re developing the solution for.
E: I’m always impressed by that last step! In my scientific approach, I write such detailed ideas and lists of behavior change strategies. And by the end of the process, Philippa has put it into a bite-size piece of content or a headline. It’s so important, because you have to engage patients quickly, maybe with a little popup and headline, and you need to encourage them to click it.
Philippa, you mentioned sending content to patients at specific times. How do you get this timing right?
P: It requires qualitative research on the patient journey so we know what the critical time points are and when specific barriers occur. We’re also developing algorithms to help better understand app usage patterns and behaviors, which allows us to use behavioral triggers to personalize delivery even more.
Aside from pushing the content at specific times, we can also provide what would be called a ‘pull’ intervention, so the content is available for the patient to consume at any time and they can choose the moment that they need it.
We can take a lot of data from the pull method and use tools such as ‘liking’ and bookmarking content to help learn what content works well and make improvements.
E: I think the combined ‘push’ and ‘pull’ approach is a patient-centric approach because it’s not just telling patients: “Here, this is what you need right now,” it is also empowering the patient to decide what content they need and when to retrieve it.
P: Yeah, this is especially true for patients who are very engaged and involved in their treatment. Some might find a push intervention too patronizing, let’s say, but they still require the same content. So having both methods creates some flexibility.
When you are developing specific programs or offerings, you are deploying them within the MyTherapy app. Why is that the approach?
P: The main benefit is the highly relevant context: MyTherapy has a huge user base across disease areas. Many patients are using the app several times a day for managing their disease. They are highly receptive to helpful content provided in the context of the app.
Also, it is truly powerful to be able to react to patients’ needs in real-time. For example, if the app detects that they have a doctor's appointment coming up, we can trigger content based on that. Finally, through MyTherapy, patients can involve other team members and connect patients with caregivers, doctors, and other people involved in managing the treatment - which allows us to engage these important stakeholders, too.
How important is the role of content within the “big picture” of a digital solution?
P: Content or information itself doesn’t drive change. We would like to think that simply providing a person with the knowledge that the treatment is good for them would instantly lead to perfect adherence, but that simply isn’t the case.
So, the provision of the information doesn’t automatically translate into action. To close that gap between information and action, content can direct to other features of the digital platform, such as prompts, cues, or access to social support. This helps influence a patient’s beliefs, motivation, and planning abilities, rather than just knowledge gaps.
Why do you believe digital solutions will become an important element in healthcare and why is behavior change key to their success?
P: A digital solution can reach an extremely wide audience, beyond what face-to-face conversations and print material can provide. When it comes to accessibility, digital interventions can counter problems patients might face in attending appointments, help fill the healthcare gap that exists in underserved areas (such as rural communities), and be translated into any language.
A digital intervention may also provide consistency in the quality of care patients are receiving, regardless of other factors.
E: For some patients, digital may also provide a higher level of comfort than addressing some topics face-to-face with an HCP. Depending on the market, this could be for reasons related to culture, gender, stigma related to a condition, and more.
Digital solutions have the potential to offer all the benefits we’ve listed, but a foundation in behavior change theory really maximizes their potential for success. And that success, on the digital frontier, can be groundbreaking. Can you tell we’re excited?
We are hiring!
Are you interested in being a part of a team at the forefront of Digital Health innovation? Check out our job ads here: Careers



